Surgical treatment of obesity
Obesity is a chronic, relapsing medical condition for which there is no "cure," only ongoing treatment which will ameliorate the condition. For obese patients, surgerical intervention is an option and is frequently the treatment of choice. Generally, the criteria include both of the following:
- Have a BMI of over 35 with obesity-related medical complications, such as high blood pressure, diabetes, elevated cholesterol, or sleep apnea.
- Have a BMI of over 40 without medical complications.
- Have been unsuccessful after undergoing appropriate medical management.
The surgical methods have changed over the years, but can be divided into gastric (stomach) restrictive procedures, wherein the quantitiy of food is "restricted" and combination restrictive/gastrointestinal bypass procedures, wherein there is a restrictive component but also a component that leads to incomplete absorption of food.
Gastric (stomach) restrictive procedures
Vertical banded gastroplasty
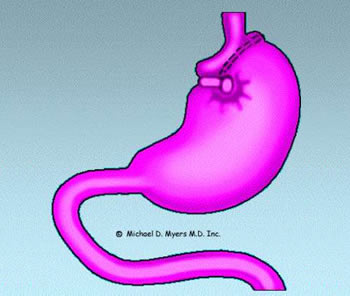 The gastric restrictive procedures are infrequently performed at this time. The
vertical banded gastroplasty (VBG), sometimes with additional reinforcement of a
small silastic (plastic) ring is one variation. In VBG, the stomach is "stapled" to
reduce its capacity to approximately 15 ml. (1/2 oz.) and a silastic ring is inserted
to help prevent the stomach from "stretching" in size. What is formed is essentially a
small stomach "pouch" that receives food from the esophagus and a much larger,
unstapled stomach that receives small amounts of food from the proximal "pouch". When
one eats, only a small amount of food can be consumed without the pouch becoming
distended. This generally leads to an early feeling of satiation or fullness. If one
continues to eat, one will develop nausea, vomiting, or pain, which generally results
in the termination of eating. Patients must adapt to their new, restricted stomach size
and restrict their food intake to prevent vomiting and pain. Complications can result
from the surgery. When gastroplasty is done by well-trained physicians, the mortality
(death rate) from the surgery is under 1 %.
The gastric restrictive procedures are infrequently performed at this time. The
vertical banded gastroplasty (VBG), sometimes with additional reinforcement of a
small silastic (plastic) ring is one variation. In VBG, the stomach is "stapled" to
reduce its capacity to approximately 15 ml. (1/2 oz.) and a silastic ring is inserted
to help prevent the stomach from "stretching" in size. What is formed is essentially a
small stomach "pouch" that receives food from the esophagus and a much larger,
unstapled stomach that receives small amounts of food from the proximal "pouch". When
one eats, only a small amount of food can be consumed without the pouch becoming
distended. This generally leads to an early feeling of satiation or fullness. If one
continues to eat, one will develop nausea, vomiting, or pain, which generally results
in the termination of eating. Patients must adapt to their new, restricted stomach size
and restrict their food intake to prevent vomiting and pain. Complications can result
from the surgery. When gastroplasty is done by well-trained physicians, the mortality
(death rate) from the surgery is under 1 %.
Complications include risk of infection, obstruction (blockage) of the outlet, necessitating surgical revision; development of blood clots in the legs or lungs; bleeding; metabolic or nutritional deficiencies (including protein calorie malnutrition); and recurrent vomiting. Although uncommon, it is possible to slowly develop vitamin (especially vitamin B-12) and mineral deficiencies resulting in anemia or osteoporosis (softening of the bones) after this surgery. Post-operatively, the patient must be followed by physicians who are familiar with the long-term complications and required long-term treatment.
The effectiveness of the surgery is fair, with loss of 40 to 50% of excess body weight with generally 50% of the weight loss being maintained after 5 years. It is common for the body weight to slowly increase after the first or second year.
The surgery requires a modified diet to prevent nausea and vomiting and to help prevent other long-term side effects. Additionally, one can (partially) bypass the "restriction" by eating calorie-dense liquids such as ice cream or regular soda. Long-term changes in eating habits must take place in order for the surgery to be successful. Vertical Banded Gastroplasty, however, is a viable treatment alternative for obese individuals.
Gastric banding
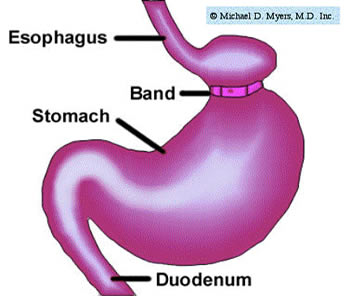 Another restrictive gastric approach is laparoscopic gastric banding. This
procedure, which was approved in the U.S. in June 2001, is popular since it is "high
tech" (utilizes a laparoscope, an instrument which is inserted into the abdominal
cavity) and recovery time is only a few days. Basically, an adjustable band is placed
around the upper portion of the stomach, resulting in (essentially) a much smaller
stomach. This restricts the amount of food that can be eaten, similar to the
vertical banded gastroplasty (see above).
Another restrictive gastric approach is laparoscopic gastric banding. This
procedure, which was approved in the U.S. in June 2001, is popular since it is "high
tech" (utilizes a laparoscope, an instrument which is inserted into the abdominal
cavity) and recovery time is only a few days. Basically, an adjustable band is placed
around the upper portion of the stomach, resulting in (essentially) a much smaller
stomach. This restricts the amount of food that can be eaten, similar to the
vertical banded gastroplasty (see above).
The European literature (where the procedure has been performed for a longer period of time) shows that weight loss is similar to that seen with vertical banded gastroplasty. Clinicians in the U.S. report less weight loss than our European colleagues. Complications include band slippage, erosion of the band into the stomach, dilation of the esophagus, and infections, many of which require removal of the device.
Surgical Results, Complications, and Nutritional Deficiencies:
Mean estimated excess body weight loss and complications from a study published in Obesity Research 2008 are as follows:
- At 7 years: < 50% of excess body weight lost
- At 9 years: < 40 % of excess body weight lost
Major late complications related to this specific surgery:
- Band eroding into the stomach: 3.3%
- Slippage: 6.5 %
- Leakage: 9.8%
- Major reoperation: 24.4%
Nutritional Deficiencies from Gastric Banding:
- Rarely significant nutritional deficiencies from the surgery itself
- Thiamine deficiency if persistent vomiting
- Occasional protein deficiency from "induced" dietary changes
The lap band is, in essence, a variation of an old surgery (gastric banding) that was abandoned in the 1980's because of a high incidence of complications (bleeding and obstruction). This newer approach is less invasive than the "old" banding procedure and the band can be adjusted (tightened or loosened) as appropriate. Many clinicans recommend this procedure for older individual (60-65 years old) who would otherwise not be a candidate for surgical intervention.
Combination restrictive/malabsorptive procedures
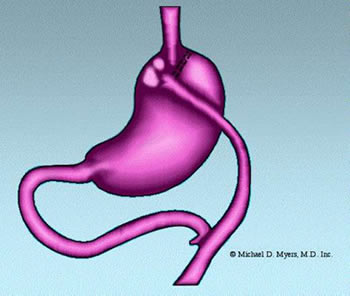 Arguably, the "gold standard" in obesity surgery is the Roux-en-Y Gastric
Bypass. This procedure involves both a "restrictive" procedure by decreasing the
size of the stomach by stapling across the top of it and a "malabsorptinve" component,
achieved by bringing-up and attaching a portion of the small intestine directly to the
stomach (thus "bypassing" part of the small intestine ). This surgery is much better
tolerated than the "old" intestinal bypass surgeries done in the 1960s and early 1970s
, but still results in significant nutritional deficiencis long-term (see below).
Arguably, the "gold standard" in obesity surgery is the Roux-en-Y Gastric
Bypass. This procedure involves both a "restrictive" procedure by decreasing the
size of the stomach by stapling across the top of it and a "malabsorptinve" component,
achieved by bringing-up and attaching a portion of the small intestine directly to the
stomach (thus "bypassing" part of the small intestine ). This surgery is much better
tolerated than the "old" intestinal bypass surgeries done in the 1960s and early 1970s
, but still results in significant nutritional deficiencis long-term (see below).
There is usually only mild malabsorption of nutrients (as compared to the old intestinal bypass surgery). This surgery causes gastrointestinal hormonal changes, which result in decreased hunger and improved satiety or fullness. Individuals undergoing this surgery will lose significant amounts of weight (mainly body fat as opposed to lean body mass or muscle tissue). Weight maintenance is generally excellent with small increases in weight occurring over subsequent years. Like any obesity surgery, the patient will require lifelong medical follow-up and treatment of the medical complications that usually occur, especially the vitamin B12 deficiency and anemia.
Surgical Results, Complications, and Nutritional Deficiencies (reference: Gastroenterology. 2002 Sep;123(3):882-932):
Mean estimated excess body weight loss and complications:
- At 2 years: approximately 66% of exces body weight lost
- At 10 years: > 50 % of exces body weight lost
Major complications related to this specific surgery:
- Marginal Ulcers at the site of anastomosis ("attachment") of the intestine to the stomach
- Stomal stenosis ("narrowing") at the stomach outlet, resulting in nausea and vomiting
- Leakage of intestinal contents
- Stomach staple line disruption resulting in the ability to consume large volumes of food
- "Dumping Syndrome" wherein consumption of food (especially carbohydrates) results in nausea, vomiting, diarrhea, abdominal pain, flushing, rapid heart beats.
Nutritional Deficiencies from Roux-en-Y Gastric Bypass:
- Iron
- Vitamin B12
- Folate
- Vitamin D
- Calcium
- Thiamine
- Protein
This procedure is now usually laparoscopically, which offers a faster surgical recovery, but with the potential for more severe surgical complications.
For more information you can watch a video outlining the procedure.
Biliopancreatic bypass procedures (and similar extensive intestinal bypass procedures)
In these procedures, the digestive juices from the liver and pancreas are diverted to the distal small intestine near the entrance to the large intestine. Thus, food enters the stomach, rapidly transverses the distal small intestine (where absorption of nutrients primarily occurs), and is then delivered to the large intestine (where excess water from the stool is removed). This results in marked malabsorption of nutrients with subsequent marked weight loss (up to 80% of excess body weight). Since there is marked malabsorption of essential nutrients, the probability of vitamin, mineral, and protein-calorie malnutrition is significant. These procedures are generally best avoided since the marked nutrient malabsorption can result in severe long-term complications.
Updated: 27 December 2011
Copyright © 1996 -2011 Michael D. Myers, M.D., Inc.
All rights reserved.
Disclaimer Statement
The above information is for general purposes only and should not be construed as definitive or binding medical advice, diagnosis or treatment. Because each person is medically different, individuals should consult their own personal physicians for specific information and/or treatment recommendations.
